U.S. Dementia-Linked Death Rate More Than Doubles (from WebMD)
Dementia is now one of the leading killers in the United States, with the rate of deaths linked to the disease more than doubling over the past two decades.
“Overall, age-adjusted death rates for dementia increased from 30.5 deaths per 100,000 in 2000 to 66.7 in 2017,” say a team of researchers from the U.S. Centers for Disease Control and Prevention.
In sheer numbers, the new analysis of death certificate data shows that dementia was noted as the primary cause for nearly 262,000 deaths in 2017, with 46 percent of those deaths due to Alzheimer’s disease.
That’s up from about 84,000 deaths attributed to dementia in 2000.
Shocking Study Finds Decreased Proteins – Not Amyloid Plaques – Cause Alzheimer’s Disease (new study 2022)

Diet and Dementia: Study Uncovers Gut-Brain Link to Alzheimer’s
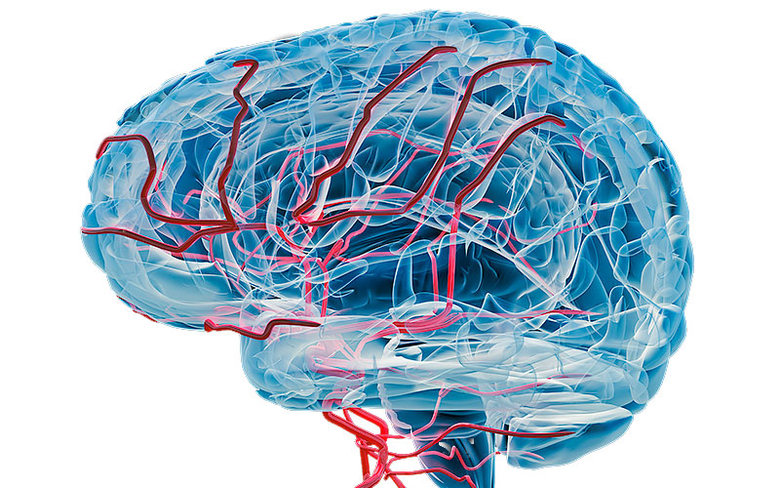
What Causes Dementia?
The most common causes of dementia include:
- Degenerative neurological diseases. These include Alzheimer’s disease, Parkinson’s disease, Huntington’s disease, and some types of multiple sclerosis. These diseases get worse over time.
- Vascular disorders. These are disorders that affect the blood circulation in your brain.
- Traumatic brain injuries caused by car accidents, falls, concussions, etc.
- Infections of the central nervous system. These include meningitis, HIV, and Creutzfeldt-Jakob disease.
- Long-time alcohol or drug use
- Certain types of hydrocephalus, a buildup of fluid in the brain
Types of Dementia
Dementia can be split into two groups based on which part of the brain is affected.
- Cortical dementias happen because of problems in the cerebral cortex, the outer layer of the brain. They play a critical role in memory and language. People with these types of dementia usually have severe memory loss and can’t remember words or understand language. Alzheimer’s and Creutzfeldt-Jakob disease are two forms of cortical dementia.
- Subcortical dementias happen because of problems in the parts of the brain beneath the cortex. People with subcortical dementias tend to show changes in their speed of thinking and ability to start activities. Usually, people with subcortical dementia don’t have forgetfulness and language problems. Parkinson’s disease, Huntington’s disease, and HIV can cause these types of dementia.
Some types of dementia affect both parts of the brain.
Are There Treatments for Dementia?
New treatment could stop dementia’s damage to the brain – study
Promising New Dementia Treatment Discovered: Sodium Selenate
To treat dementia, doctors will treat whatever is causing it. About 20% of the causes of dementia are reversible.
Causes of dementia that may be reversible include:
- Alcohol or drug abuse
- Tumors
- Subdural hematomas, blood clots beneath the outer covering of the brain
- Normal-pressure hydrocephalus, a buildup of fluid in the brain
- Metabolic disorders such as a vitamin B12 deficiency
- Low levels of thyroidhormones, called hypothyroidism
- Low blood sugar, called hypoglycemia
- HIV-associated neurocognitive disorders (HAND)
These forms of dementia are partially manageable, but they aren’t reversible and get worse over time:
- Alzheimer’s disease
- Vascular dementia
- Dementia from Parkinson’s disease and similar disorders
- Dementia with Lewy bodies
- Frontotemporal dementia (Pick’s disease)
- Creutzfeldt-Jakob disease
What Are the Stages of Dementia?
Usually, dementia goes through these stages. But it may vary depending on the area of the brain that is affected.
1) No impairment: Someone at this stage will show no symptoms, but tests may reveal a problem.
2) Very mild decline: You may notice slight changes in behavior, but your loved one will still be independent.
3) Mild decline: You’ll notice more changes in his thinking and reasoning. He may have trouble making plans, and he may repeat himself a lot. He may also have a hard time remembering recent events.
4) Moderate decline: He’ll have more problems with making plans and remembering recent events. He may have a hard time with traveling and handling money.
5) Moderately severe decline: He may not remember his phone number or his grandchildren’s names.He may be confused about the time of day or day of the week. At this point, he will need assistance with some basic day-to-day functions, such as picking out clothes to wear.
6) Severe decline: He’ll begin to forget the name of his spouse. He’ll need help going to the restroom and eating. You may also see changes in his personality and emotions.
7) Very severe decline: He can no longer speak this thoughts. He can’t walk and will spend most of his time in bed.
How Common Is Dementia?
About 5% to 8% of adults over age 65 have some form of dementia. This percentage doubles every 5 years after 65. As many as half of people in their 80s have some dementia.
Ultrasound waves applied to the whole brain improve cognitive dysfunction in mice with conditions simulating vascular dementia and Alzheimer’s disease. The research, conducted by scientists at Tohoku University in Japan, suggests that this type of therapy may also benefit humans.
The team, led by cardiologist Hiroaki Shimokawa, found that applying low-intensity pulsed ultrasound (LIPUS) to the whole brain of the mice improved blood vessel formation and nerve cell regeneration without having obvious side effects.
“The LIPUS therapy is a non-invasive physiotherapy that could apply to high-risk elderly patients without the need for surgery or anaesthesia, and could be used repeatedly,” says Shimokawa.
Dementia affects about 50 million people worldwide, with 10 million new cases occurring every year. But there are currently no curative treatments available for vascular dementia or Alzheimer’s disease, the most common causes of dementia. Also, the cells lining the brain’s blood vessels are tightly packed, forming a blood-brain barrier that prevents large molecules from crossing into the brain tissue. This limits the types of drugs and cell therapies that could be made available to treat dementia.
Shimokawa and his team had conducted previous studies showing that LIPUS improved blood vessel formation in pigs with myocardial ischemia, a condition where there is reduced blood flow to the heart. Other studies have reported that LIPUS increases the production of proteins involved in nerve cell survival and growth, in addition to a role in promoting nerve regeneration. Focusing LIPUS treatment on a region in the brain called the hippocampus, which is involved in memory, has also been found to improve dementia in mice, but the details of how it does this need to be more fully investigated.
The Tohoku University team wanted to find out if whole-brain rather than focused LIPUS is effective in treating mouse models of dementia, and if it was, what was happening at the molecular levels to achieve this.
They found that cognitive impairment markedly improved in mice with conditions similar to vascular dementia and Alzheimer’s disease when LIPUS was applied to the whole brain three times a day for 20 minutes each time. The mice with vascular dementia received the treatment on the first, third and fifth days following a surgical procedure that limited the brain’s blood supply. The mice with a condition simulating Alzheimer’s disease in humans received 11 LIPUS treatments over a period of three months.
At the molecular level, genes related to the cells lining blood vessels were turned on. Also, there was increased expression of an enzyme involved in blood vessel formation and a protein involved in nerve cell survival and growth.
The researchers conclude that their study, recently published in the journal Brain Stimulation, provides the first experimental evidence that whole-brain LIPUS therapy markedly improves cognitive dysfunctions without serious side effects by enhancing specific cells related to dementia’s pathology.
The first clinical trials to evaluate the effectiveness and safety of the LIPUS treatment are already underway.
Shocking Study Finds Decreased Proteins – Not Amyloid Plaques – Cause Alzheimer’s Disease (new study 2022)
Unraveling Alzheimer’s Mystery: Rare Gene Variant Offers New Hope for Treatment : https://neurosciencenews.com/neuroprotective-alzheimers-gene-23240/
The researchers describe Reelin as a “cousin” of the more famous APOE. Both Reelin and APOE compete to bind to similar cellular receptors, essentially jostling to occupy the same seat.
When Reelin sits in the receptor seat, it diminishes the phosphorylation of tau, a protein known to form pathological tangles in brains with Alzheimer’s disease. When APOE binds the receptor, it has the opposite effect.
Reelin is a protein with a pivotal role in the regulation of brain cell development and function. In fact, previous reports have linked mutations in Reelin to diseases like autism, schizophrenia, epilepsy, and bipolar disorder. https://neurosciencenews.com/neuroprotective-alzheimers-gene-23240/