This is not a definitive resource and the rules for CPR (Cardio-Pulmonary Resuscitation) and BLS (Basic Life Support) are always evolving. This information is being taken from various sources for your entertainment and should not replace professional instruction or certification. Please use this information to help broaden your understanding of a complex and critical emergency situation that you may find yourself in. THANK YOU for wanting to know more about how to be helpful in emergency situations. Remember: CALL 911 should you EVER respond or witness a life threatening emergency.
According to the Centers for Disease Control (CDC), heart disease continues to be the leading cause of death in the United States and is responsible for over 600,000 deaths every year. Research continues to improve how we respond with life-saving techniques to emergencies. These techniques are based on the most current research and are organized into a systematic response called the Chain of Survival, which begins with Basic Life Support (BLS). The Chain of Survival provides the victim the best chance to receive the care needed and return to a healthy life.
The heart pumps blood through the lungs, where blood takes in oxygen and releases carbon dioxide. This blood then returns to the heart where it is pumped out to vital organs—the heart and brain—as well as the rest of the body. When the heart stops, blood flow stops, and the person quickly becomes unconscious. Without blood flow, the heart and the brain quickly become damaged due to a lack of oxygen. The actions that make up BLS try to prevent or slow the damage until the cause of the problem can be corrected. BLS improves a person’s chance of surviving until advanced care becomes available.
Taking the right action quickly and confidently can make the difference between life and death for a person dealing with cardiac arrest.
Keys for BLS:
- Quickly start the Chain of Survival.
- Deliver high-quality chest compressions to circulate oxygen to the brain and vital organs.
- Know when and how to use an Automated External Defibrillator (AED).
- Provide rescue breathing.
- Understand how to work with other rescuers as part of a team.
- Know how to treat choking.
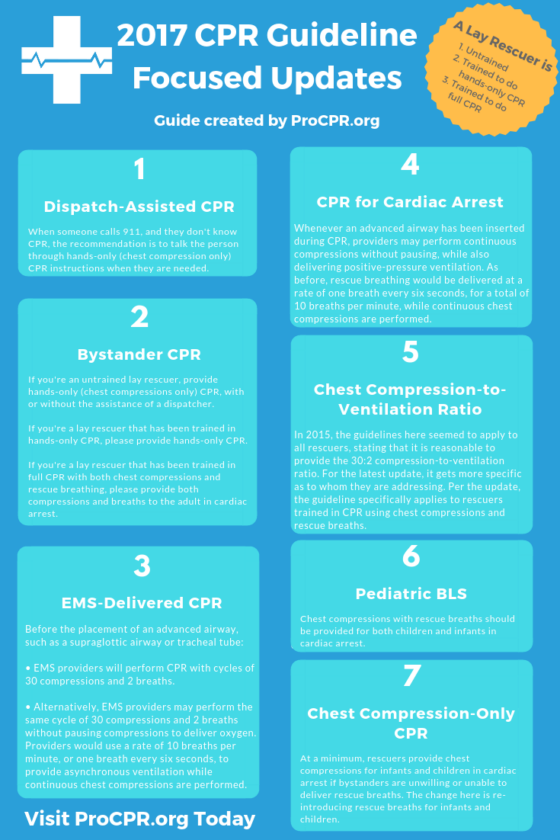
7 changes which include some clarifications on the descriptions of lay rescuers*.
Nursing with Professor B
- Dispatch-Assisted CPR (for adults in out-of-hospital cardiac arrest)When someone calls 911, and they don’t know CPR, they’ll often be directed on what to do over the phone by dispatch. Since chest compressions are pretty simple to teach verbally, the recommendation is to talk the person through hands-only (chest compression only) CPR instructions. Keep in mind that this is the recommendation for adults with a suspected out-of-hospital cardiac arrest (OHCA). The change from the 2015 guidelines is the addition to provide the instructions when they are needed.
- Bystander CPR (for adults in out-of-hospital cardiac arrest)If you’re an untrained lay rescuer, provide hands-only (chest compressions only) CPR, with or without the assistance of a dispatcher.If you’re a lay rescuer that has been trained in hands-only CPR, please provide hands-only CPR.If you’re a lay rescuer that has been trained in full CPR with both chest compressions and rescue breathing, please provide both compressions and breaths.The change from 2015 is more clarification of what we had before, with the addition of the above recommendation for a lay-rescuer that has been trained in hands-only CPR.It is important that all lay rescuers know that you don’t need to have taken a CPR class to be able to do chest compressions. A CPR certification card is not like a license to drive. It is meant to certify that you were taught a subject matter.
- EMS-Delivered CPR (before placement of an advanced airway)Before the placement of an advanced airway, such as a supraglottic airway or tracheal tube:• EMS providers will perform CPR with cycles of 30 compressions and 2 breaths.• Alternatively, EMS providers may perform the same cycle of 30 compressions and 2 breaths without pausing compressions to deliver oxygen. Providers would use a rate of 10 breaths per minute, or one breath every six seconds, to provide asynchronous ventilation while continuous chest compressions are performed.These updates do not preclude the 2015 recommendation for EMS systems that have adopted bundles of care, that a reasonable alternative is the minimal interruption of chest compressions for witnessed, shockable, out-of-hospital cardiac arrest.The change from 2015 is based on the use of interrupted vs continuous chest compressions when EMS providers performed CPR using both rescue breathing and chest compressions prior to placement of an advanced airway. The recommendation had been to pause between the cycles of 30 compressions to deliver two breaths, delivering each for one second.
- CPR for Cardiac Arrest (when an advanced airway is inserted during CPR)Whenever an advanced airway has been inserted during CPR, providers may perform continuous compressions without pausing, while also delivering positive-pressure ventilation. As before, rescue breathing would be delivered at a rate of one breath every six seconds, for a total of 10 breaths per minute, while continuous chest compressions are performed.This change seems like more of a clarification in the language. The 2015 guidelines started out with rescuers no longer delivering the cycles of 30 compressions and 2 breaths (ie, no longer interrupting compressions to give those two breaths). It continued with the same recommendation of 10 breaths per minute while continuous chest compressions are performed. This change seems to clarify that CPR is not stopped, rather it is enhanced by the continuous chest compressions.
- Chest Compression-to-Ventilation Ratio (for adults in cardiac arrest)In 2015, the guidelines here seemed to apply to all rescuers, stating that it is reasonable to provide the 30:2 compression-to-ventilation ratio. For the latest update, it gets more specific as to whom they are addressing. Per the update, the guideline specifically applies to rescuers trained in CPR using chest compressions and rescue breaths.
- Components of High-Quality CPR: Pediatric BLS (for infants and children in cardiac arrest)Chest compressions with rescue breaths should be provided for both children and infants in cardiac arrest. Since the release of the 2015 guidelines, evidence has pointed toward providing full CPR with both chest compressions and rescue breaths. The old guideline wasn’t specific and only mentioned that conventional CPR should be provided for pediatric cardiac arrests.
- Components of High-Quality CPR: Chest Compression-Only CPR (for infants and children)The latest update recommends that, at a minimum, rescuers provide chest compressions for infants and children in cardiac arrest if bystanders are unwilling or unable to deliver rescue breaths. The change here is re-introducing rescue breaths for infants and children.The 2015 guideline recommendation aligned the adult recommendation for hands-only CPR with the recommendation for children and infants, but the benefit of rescue breaths have justified a different recommendation for children and infants.In other words, if you can provide rescue breaths alongside chest compressions for children and infants, do it. If you are unwilling or unable to provide rescue breaths, then at least do the chest compressions.
*A lay rescuer is described as someone that is:
- Untrained
- Trained to do hands-only CPR (doing only chest compressions)
- Trained to do full CPR including both chest compressions and rescue breathing
Here’s a PDF of the highlights from the AHA (2020).
TEDx Talks
Sudden Cardiac Arrest
Also known as Cardiac Arrest, Sudden Cardiac Death www.nhlbi.nih.gov/
Emergency Treatment
Sudden cardiac arrest (SCA) is an emergency. A person having SCA needs to be treated with a defibrillator right away. This device sends an electric shock to the heart. The electric shock can restore a normal rhythm to a heart that’s stopped beating.
To work well, defibrillation must be done within minutes of SCA. With every minute that passes, the chances of surviving SCA drop rapidly.
Police, emergency medical technicians, and other first responders usually are trained and equipped to use a defibrillator. Call 9–1–1 right away if someone has signs or symptoms of SCA. The sooner you call for help, the sooner lifesaving treatment can begin.
Automated External Defibrillators
Automated external defibrillators (AEDs) are special defibrillators that untrained bystanders can use. These portable devices often are found in public places, such as shopping malls, golf courses, businesses, airports, airplanes, casinos, convention centers, hotels, sports venues, and schools.
AEDs are programmed to give an electric shock if they detect a dangerous arrhythmia, such as ventricular fibrillation. This prevents giving a shock to someone who may have fainted but isn’t having SCA.
You should give cardiopulmonary resuscitation (CPR) to a person having SCA until defibrillation can be done.
People who are at risk for SCA may want to consider having an AED at home. A 2008 study by the National Heart, Lung, and Blood Institute and the National Institutes of Health found that AEDs in the home are safe and effective.
Some people feel that placing these devices in homes will save many lives because many SCAs occur at home. Others note that no evidence supports the idea that home-use AEDs save more lives. These people fear that people who have AEDs in their homes will delay calling for help during an emergency. They’re also concerned that people who have home-use AEDs will not properly maintain the devices or forget where they are.
When considering a home-use AED, talk with your doctor. He or she can help you decide whether having an AED in your home will benefit you.
Treatment in a Hospital
If you survive SCA, you’ll likely be admitted to a hospital for ongoing care and treatment. In the hospital, your medical team will closely watch your heart. They may give you medicines to try to reduce the risk of another SCA.
While in the hospital, your medical team will try to find out what caused your SCA. If you’re diagnosed with ischemic heart disease, you may have percutaneous coronary intervention, also known as coronary angioplasty, or coronary artery bypass grafting. These procedures help restore blood flow through narrowed or blocked coronary arteries.
Often, people who have SCA get a device called an implantable cardioverter defibrillator (ICD). This small device is surgically placed under the skin in your chest or abdomen. An ICD uses electric pulses or shocks to help control dangerous arrhythmias.
What are the risk factors of sudden cardiac arrest?
There are many factors that can increase a person’s risk of sudden cardiac arrest and sudden cardiac death.
The two leading risk factors include:
- Previous heart attack (75 percent of SCD cases are linked to a previous heart attack) -A person’s risk of SCD is higher during the first six months after a heart attack.
- Coronary artery disease (80 percent of SCD cases are linked with this disease) -Risk factors for coronary artery disease include smoking, family history of cardiovascular disease, high cholesterol or an enlarged heart.
Other risk factors include:
- Ejection fraction of less than 40 percent, combined with ventricular tachycardia (see information below about EF)
- Prior episode of sudden cardiac arrest
- Family history of sudden cardiac arrest or SCD
- Personal or family history of certain abnormal heart rhythms, including long QT syndrome, Wolff-Parkinson-White syndrome, extremely low heart rates or heart block
- Ventricular tachycardia or ventricular fibrillation after a heart attack
- History of congenital heart defects or blood vessel abnormalities
- History of syncope (fainting episodes of unknown cause)
- Heart failure: a condition in which the heart’s pumping power is weaker than normal. Patients with heart failure are 6 to 9 times more likely than the general population to experience ventricular arrhythmias that can lead to sudden cardiac arrest.
- Dilated cardiomyopathy (cause of SCD in about 10 percent of the cases): a decrease in the heart’s ability to pump blood due to an enlarged (dilated) and weakened left ventricle
- Hypertrophic cardiomyopathy: a thickened heart muscle that especially affects the ventricles
- Significant changes in blood levels of potassium and magnesium (from using diuretics, for example), even if there is not organic heart disease
- Obesity
- Diabetes
- Recreational drug abuse
- Taking drugs that are “pro-arrhythmic” may increase the risk for life-threatening arrhythmias
Sudden cardiac death (SCD) occurs rarely in athletes or young people, but when it does happen, it often affects us with shock and disbelief.
PulsePoint Respond is a 911-connected app that can immediately inform you of emergencies occurring in your community and can request your help when CPR is needed nearby. PulsePoint Respond is not available in all areas. The service is only offered where adopted by the local public safety agency.
PulsePoint AED is a simple-to-use tool that enables you to help build the public AED registry in your community – or anywhere!
PulsePoint is a 501(c)(3) public non-profit foundation building applications that help public safety agencies inform and engage their citizens.